Failed Back Surgery…Why?
What causes a failed back surgery?
One answer could be an inadequate preoperative workup, before the fusion, to help identify the painful disc.
This is a situation that I’m seeing more often, as fusions are being performed more routinely for axial back pain. The gender and age vary, but the stories are often similar. The patient is experiencing chronic deep midline axial back pain that did not respond to exercise or pain management protocols. The MRI findings were similar for the L3-S1 levels with changes of disc darkening and bulging. Discography was not performed preoperatively to determine a definitive diagnosis or level(s) that were responsible for the pain. A single level fusion was performed with no benefit and slight worsening of the pain. There was no suggestion of fusion nonunion in any of the patients. What’s going on ?
The above history is typical for these patients and the only consistent finding on physical exam is recreation of the axial low back pain with pressure on the symptomatic interlaminar space (between the spinous processes) at the symptomatic level. This is a key physical finding.
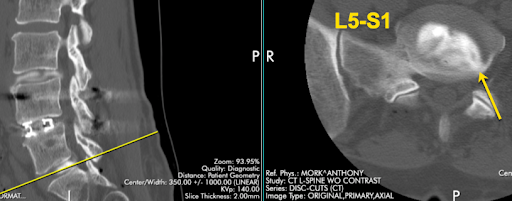
The cause of the deep axial low back pain is shown by the CT discogram above. There is obvious annular tearing of the L5-S1 disc, further confirmed with concordant affirmation during the provocative portion of the test. Although there was annular tearing at L3-4, it was not concordant or very painful (2-3/10).
This person was treated with a transforaminal discectomy (Transforaminal 1 Course at the L5-S1 level with about 90% relief of axial back pain. There were no complications and the recovery was short.
This case makes a couple of other interesting points. The first is that doing a provocative discogram before the fusion might have helped identify the painful disc and the best level to fuse. Complicating this suggestion is the fact that medicare and most payors are no longer reimbursing for discography, which is unfortunate. The prolonged pain, suffering and additional procedures this patient endured by not having the correct diagnosis in the beginning, might make some patients consider paying cash for a discogram “just to be sure”.
From a business standpoint, since there is no insurance reimbursement, this could be your first step into a cash or “hybrid” practice.
The second point to make is to consider doing a transforaminal discectomy yourself (Transforaminal 1 Course) as a first step. It gave this patient 90% relief at almost 1 year post op.
Why do a fusion, when a transforaminal discectomy might be all that’s needed. I’m a firm believer of “progression of treatment” and I think it makes a lot more sense to do a lesser procedure first and then do more later, if necessary.
Onward and Upward
Tony Mork, MD
Endoscopic Spine Specialist